Contrast Enhancement: Expanding Frontiers of Ultrasound
Contrast enhanced agents have been key to enhancing the diagnostic capability of computed tomography (CT), magnetic resonance imaging (MRI) and clinical radiography. Since the turn of the millennium, contrast enhancement for ultrasound (CEUS) has also emerged as an imaging tool. Along with developments in scanning hardware, new contrast agents have expanded the application envelope of ultrasound. During CEUS, tiny liquid suspensions of biodegradable gas-filled microspheres (also known as ‘microbubbles’) are injected as tracer for microscopic ultrasound imaging examinations. The microbubbles are metabolized and expelled from the body within minutes. Clinical applications for ultrasound contrast agents potentially extend to any organ or physiological system that is evaluated with conventional ultrasound, with the singular exception of the fetus. As of now, major applications are in cardiac and hepatic imaging. Other applications are being explored, including paediatric CEUS.
From imaging complement to alternative
There is growing evidence that CEUS is valuable, accurate and cost-effective. It often complements CT and MRI, and in several instances, has become an important alternative to either. This especially concerns patients with renal failure, those who wish to avoid the radiation risk of CT or cannot cope with being shut inside a scanner.
Interest in CEUS has grown sharply since 2016, after the Food and Drug Administration (FDA) approved a microbubble contrast agent for liver CEUS, paving the way for much faster growth in the US market.
The microvascular challenge
Clinically, one of the key drivers for CEUS has been limits to the performance of ultrasound imaging and Doppler techniques. While B-Mode provides anatomical information, Doppler allows for visualization of the larger vessels in the macrovascular system, based on the velocity of blood flow in the intravascular lumen. However, there are limits to both spatial resolution and Doppler sensitivity.
The utility of conventional ultrasound reduces rapidly when a clinician needs to visualise smaller vessels and capillaries, lying within deeper structures of the body’s microvascular system.
To achieve this, and more specifically, determine differences in arrival-, dwell- and wash-out time within specific regions of parenchymal tissue, there is a need for direct imaging via tracers. It is in this capacity that contrast agents play a useful role. They improve the sensitivity and specificity of ultrasound and greatly expand its scope for application.
The advantages of CEUS
CEUS has certain intrinsic advantages when compared to other imaging modalities.
It permits ultra-high temporal imaging of contrast enhancement profiles at between 20 and 50 images per second, for a duration of about 5-8 minutes. This makes it possible for continuous visualization of images in all phases – from the early arterial to the late phase – and seek to ensure no patterns are missed. CEUS also allows for both follow-up examinations at short intervals, and, given its lack of ionising radiation, for repeated examinations over a long period of time – a common requirement for chronic diseases. CEUS is also convenient. It can be used at multiple bedsite locations – from intensive care units (ICUs) and operating rooms to recovery rooms and ambulatory units.
Contrast agents for ultrasound have been found to be safe with no cardio-, hepato-, or nephro-toxic effects. Laboratory checks to assess liver, renal or thyroid function before administration are therefore not required.
Evaluating liver lesions
In the liver, CEUS has proven its utility when clinicians encounter focal lesions during cross-sectional imaging of an asymptomatic patient. Though most such collateral encounters are benign, it is necessary to pursue dedicated imaging characterization and diagnosis, in order to exclude malignancy. This is especially true when the lesions are large or otherwise atypical and when the patient is from a high-risk group.
Traditionally, the evaluation of lesions was undertaken with magnetic resonance imaging (MRI) or multiphase CT. However, the former was generally limited in availability, while multiphase CT invoked concerns about radiation. CEUS is seen to be safe, non-invasive and available.
When CEUS is used in the liver, microbubble delivery occurs via two routes, namely the hepatic artery and portal vein. Blood flow through the latter needs to first transit gastrointestinal circulation, and therefore arrives at a later time point. This permits differentiation between the two wash-in phases.
CEUS enhances the display of vascularity in liver lesions, and is both accurate and reproducible. The vascular supply for focal liver lesions is characteristic of a particular lesion type and different from normal liver tissue. While abnormal vascularity of hepatocellular carcinoma can be demonstrated early during the contrast inflow phase, metastases are characterised in the late phase. In addition, the timing and the intensity of washout can differentiate hepatocellular malignancies from non-hepatocellular ones. The former demonstrate delayed and weak washout. Non-hepatocellular tumours show strong, early washout.
The need for right dosing
Using the optimal dose is important. Too high a contrast agent dose results in artefacts, particularly in the early phases of enhancement. These include acoustic shadowing, over-enhancement of small structures and signal saturation, which is also detrimental for quantification.
On the other hand, a low dosage causes the concentration of microbubbles to be sub-diagnostic in the late phase, challenging the detection of wash out.
If the wash out is early, the dose was probably too low. Here, it can be important to evaluate the status of the liver as being healthy or diseased. In difficult cases, a second (higher) dose may be administered, with no or only limited scanning in the early phases to reduce bubble destruction. The exact dose depends on the contrast agent, ultrasound equipment (software version, transducer), type of examination, organ and target lesion, size and age of the patient.
Other challenges for CEUS in the liver
Apart from the challenge of dosing, there are other limitations too in the use of CEUS in the liver. Very small lesions may be overlooked. The smallest detectable lesions are considered to be 3-5 mm in diameter.
There are also some specific shortcomings, such as fat layers surrounding the falciform ligament. These can cause enhancement defects which might be confused with a lesion.
Given limits to penetration, deep-seated lesions may also not always be accessible. However, some clinicians suggest that bringing the liver closer to the transducer via use of left lateral decubitus positioning can overcome such a limitation.
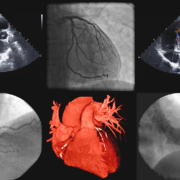
CEUS and cardiology
CEUS has also shown remarkable utility in cardiology. After the tracer injection, micro-bubbles follow the flow and distribution of red blood cells. opacify the cardiac chambers and enhance delineation of the left ventricular border. The microbubbles are then ejected into the arterial circulatory system, allowing for visualization of blood flow into the parenchymal organs.
An assessment of cardiac function depends on proper delineation of the endocardial border and wall motion patterns. This is where conventional ultrasound faces serious limits. Intracardiac echo reflections couple to weak signals from structures in parallel to the echo beam. The ensuing delineation of the endocardial border can therefore be unclear, resulting in an inaccurate left ventricle assessment.
What contrast agents achieve here is to completely fill the ventricular cavity, and thereby delineate it in a similar fashion to cardiac MRI.
Proper assessment of cardiac function is especially important for stress echo tests in order to demonstrate inducible ischaemia. Here, the risk of a stress examination means that inadequate image quality is unacceptable. In addition, precise delineation of the cardiac chamber is required to make an assessment of heart insufficiency and decide on whether an automatic implantable cardioverter defibrillator (AICD) is indicated. Such precision is also required with cancer chemotherapy patients, in order to assess cardiotoxicity.
New contrast agents
First-generation ultrasound contrast agents were based on air, which was sufficiently soluble in blood for use with the equipment of the time. Second-generation agents contain an inert lipophilic gas with very low solubility, thus avoiding early leakage of the gas. This provides more stability to the microbubbles.
Modern contrast agents have a shell made out of a thin and flexible phospholipid membrane. One side, which faces the surrounding blood, has hydrophilic properties. On the other, lipophilic chains make contact with the encapsulated gas.
Over recent years, technology development has focused on ultrasound contrast agents which reduce microbubble size and increase persistence within the blood in the circulatory system, to 10 or more minutes. Researchers are also seeking to develop new materials and gases to control the encapsulating shell or surface of the microbubble, in order to inhibit dissolution and diffusion.
Constraints faced by microbubbles
In spite of the above developments, there are some constraints with microbubbles.
They do not last long in circulation, due to being taken up by immune system cells, the liver or spleen. They also have low adhesion efficiency, which means only a small fraction bind to an area of interest. Microbubbles can also burst at low ultrasound frequencies and at high mechanical indices, which, in turn, can lead to local microvasculature ruptures and haemolysis.
Guidelines on CEUS
The use of CEUS varies widely from one country to another, and even between different healthcare facilities in the same country.
Guidelines were first issued for the use of CEUS for liver applications in 2004. They were updated in 2008, reflecting growth in the availability of contrast agents. CEUS has also been recommended in guidelines for several non-liver applications, under the auspices of EFSUMB.
The latest guidelines date to 2012. They are published under the auspices of the World Federation for Ultrasound in Medicine and Biology (WFUMB) and the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB). The aim is to create standard protocols for CEUS in liver applications across the world.
According to the guidelines, CEUS is indicated for liver lesion characterization in the following clinical situations:
• Incidental findings on routine ultrasound
• Lesion(s) or suspected lesion(s) detected with US in patients with a known history of a malignancy, as an alternative to CT or MRI
• Need for a contrast study when CT and MRI contrast are contraindicated
• Inconclusive MRI/CT
• Inconclusive cytology/histology results
Paediatric applications
One new frontier for CEUS applications consist of children.
Currently, sulphur hexafluoride gas microbubbles have been approved by the FDA in the US for characterising focal liver lesions in children and vesico-ureteral reflux. In Europe, CEUS in children is indicated for vesico-ureteral reflux, although there is
significant off-label use too.